If you’re an adult taking diuretic medications, you know that staying hydrated can feel like a balancing act. These “water pills” are commonly prescribed for conditions like high blood pressure and pulmonary edema, but they work by increasing urination—which puts you at higher risk of dehydration.
A study found that 75% of Americans do not drink enough water to stay properly hydrated. As we age, our thirst response diminishes, making it even harder to gauge when our bodies need more fluids.
But don’t let your water retention pills dry you out! We’ll discuss exactly how much water you should drink if you’re taking diuretics and provide some practical tips for incorporating sufficient hydration into your daily routine.
With the right knowledge and a proactive approach, you can stay healthy, hydrated, and feeling your best while taking these important medications.
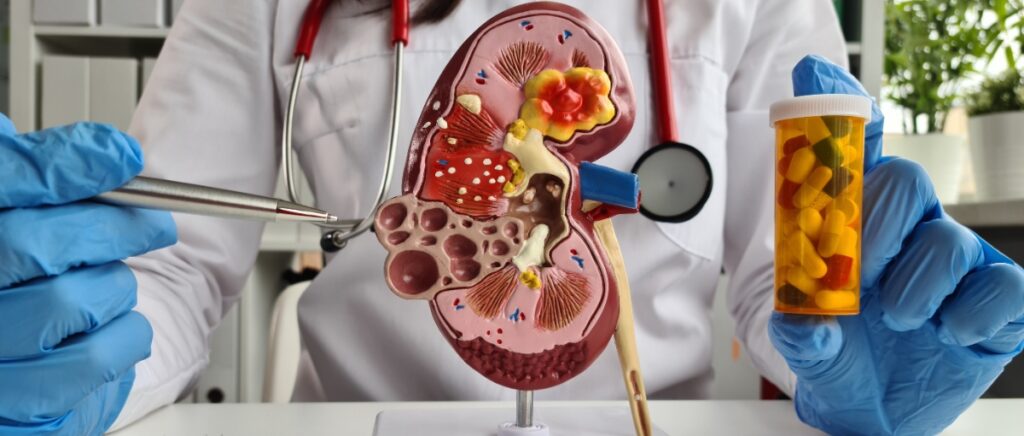
What Are Diuretics?
Diuretics, commonly known as “water pills,” are medications that help the body eliminate extra fluid and salt through increased urine production. They work by signaling the kidneys to flush out more water and salt, which exits the body when you urinate. When considering treatment options, many patients ask, “What is the best diuretic for high blood pressure?”
There are three main types of diuretic medications:
- Thiazide diuretics: One of the most commonly prescribed diuretics, and they include medicines like hydrochlorothiazide (Microzide) and chlorthalidone (Thalitone).
- Loop diuretics: These are stronger diuretics used for more severe fluid retention, and include furosemide (Lasix) and bumetanide (Bumex).
- Potassium-sparing diuretics: These are often combined with other diuretics to prevent potassium loss. They include spironolactone (Aldactone) and triamterene (Dyrenium).
According to the Mayo Clinic, doctors most often prescribe diuretics to treat conditions like:
- High blood pressure
- Edema (swelling) caused by excess fluid buildup
- Heart disease or failure
- Liver or kidney disorders
While these medications are highly effective at ridding your body of excess fluid and reducing strain on your blood vessels and heart, they can also deplete your fluid levels too much, leading to dehydration. That’s why it’s so important to monitor your fluid intake and drink enough water when taking any type of diuretic medication.
Diuretics Side Effects
While diuretics are effective, they can cause several side effects. Common issues include:
- Frequent urination
- Electrolyte imbalances (such as low potassium or sodium)
- Dehydration, leading to dizziness or muscle cramps
- Increased thirst or headaches
- Kidney dysfunction, particularly in those with pre-existing kidney conditions
How Diuretics Can Lead to Dehydration
Diuretics, also known as water pills, work by blocking the reabsorption of sodium and water in the kidneys, which increases urine production. While this helps remove excess fluid from your body, it’s essential to ask, how much water should I drink while taking water pills? Drinking too little water may cause dehydration, as these medications can flush out more fluid than your body needs. To avoid this, ensure you stay hydrated by consuming an appropriate amount of water while taking a water pill prescription.
When you lose more fluid than you take in, your body doesn’t have enough water and other fluids to carry out its normal functions. Older adults are especially susceptible to dehydration for a few reasons:
- As we age, our thirst response, stimulated by dehydration, becomes weaker, so we may not feel thirsty even when our bodies need fluids.
- Our kidneys lose some of their ability to concentrate urine and conserve water as we get older.
- Many older adults who have health conditions or take medications (like diuretics) are especially prone to dehydration risk.
It’s important to recognize the signs of dehydration, as it can sneak up on you without warning.
- Excessive thirst
- Dark-colored urine
- Fatigue
- Dizziness
- Confusion
- Dry mouth and lips
If dehydration becomes severe, it can lead to serious complications like kidney problems, seizures, and even heat stroke. According to the National Institutes of Health, dehydration is a frequent cause of hospitalization among older adults.
The good news is that dehydration is preventable—it just takes some proactive planning.
How Much Water You Should Drink
Can drinking too much water affect medication? It depends. While individual fluid needs can vary based on factors like age, climate, diet, and activity level, a general guideline for people taking diuretics is to aim for 1.5 to 2 liters, which is equal to about 6 to 8 cups of fluids per day—unless your doctor has instructed you otherwise.
Keep in mind that you may need more fluids if you:
- Live in a hot, humid climate or spend lots of time in the sun.
- Exercise regularly or participate in strenuous activities.
- Consume a diet high in salty, spicy, or sugary foods.
- Have a medical condition that causes fluid loss, like vomiting or diarrhea.
The best way to know if your water intake is enough is to pay attention to your body’s signals and check in with your doctor regularly. They can assess your individual needs and adjust your diuretic dosage or hydration plan if needed.
6 Simple Ways to Stay Hydrated on Diuretics
Drinking enough water can feel like a chore, but with a little creativity and planning, you can easily incorporate hydration into your daily routine. Here are a few simple tips:
- Carry a refillable water bottle with you wherever you go, and aim to finish a 20-ounce bottle three to four times daily.
- Set reminders on your phone or post a note on your fridge to prompt you to drink regularly throughout the day.
- Jazz up plain water with slices of fruit, mint leaves, or a splash of juice for flavor without added sugar or calories.
- Enjoy water-rich foods like watermelon, cucumber, zucchini, strawberries, and soups to boost your water intake.
- Sip on unsweetened herbal tea or sparkling water as a flavorful alternative to plain water.
- Be extra mindful of your fluid intake when exercising or spending time outdoors in hot weather—drink water before, during, and after activity.
When to Check With Your Doctor
Staying on top of your hydration is key when taking a diuretic, but sometimes, you may need extra medical advice or guidance. Reach out to your doctor if you:
- Struggle to drink enough fluids due to nausea, appetite loss, weight loss, or other symptoms.
- Experience frequent signs of dehydration like dark urine, dizziness, or fatigue.
- Have a hard time keeping fluids down due to vomiting or diarrhea.
- Feel like your medication is causing severe fluid loss or other intolerable side effects.
In addition to watching for warning signs, be sure to keep up with regular check-ups while on diuretics. Your doctor will likely order periodic blood and urine tests to monitor your kidney function and electrolyte levels and may need to adjust your dosage over time.
The Key to Hydration on Diuretics: Balance and Communication
Managing your fluid levels while taking a diuretic may feel daunting at first, but by staying mindful of your intake, listening to your body’s cues, and regularly touching base with your doctor, you can find the hydration sweet spot that keeps you feeling your best.
Remember, every person’s fluid needs are different, so what works for one may not work for all. Work closely with your healthcare team to develop a personalized hydration plan that fits your unique medical needs, lifestyle, and preferences.
With a little preparation, a lot of communication, and a dash of creativity, you can strike the perfect balance between your diuretic’s benefits and the body’s fundamental need for fluids. Drink up, and here’s to your hydration health!
Sources
Cleveland Clinic. (2021). Diuretics. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/21826-diuretics
National Center for Biotechnology Information. (2020). Loop Diuretics. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK555956/
Heart and Stroke Foundation of Canada. (n.d.). Diuretics. Heart and Stroke. https://www.heartandstroke.ca/heart-disease/treatments/medications/diuretics
National Center for Biotechnology Information. (2019). Thiazide Diuretics. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK532918/
National Center for Biotechnology Information. (2019). Potassium-Sparing Diuretics. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK546656/
Drugs.com. (n.d.). Potassium-sparing diuretics. https://www.drugs.com/drug-class/potassium-sparing-diuretics.html
Mayo Clinic. (2023). Diuretics: A cause of low potassium?. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/diuretics/art-20048129
ScienceDirect. (2017). Renal Effects of Diuretics. https://www.sciencedirect.com/science/article/abs/pii/S0031938416307235